Calcium, Phosphate, Parathyroid Hormone
Finding digestible sources of calcium can be difficult yet VITAL in the state of low metabolism.
Calcium is the most abundant mineral in our body and is involved in a large number of cellular processes. Calcium is anti-inflammatory and combats many effects of stress.
Simply put, if calcium intake isn’t sufficient in the diet or under stress, parathyroid hormone (PTH) rises, which opposes proper metabolism.
Parathyroid hormone liberates calcium from our bones into the bloodstream to maintain normal blood levels of calcium, but PTH can also cause calcium to be liberated into the soft tissues (calcification), and activate nitric oxide.
Also, when calcium is deficient in the diet, this usually means that we have an excess of phosphate. High phosphate intake (cereals, legumes, meat, and fish are rich in phosphate) lowers energy metabolism and causes inflammation and activates PTH.
Striving for a calcium to phosphate ratio above 1:1 is essential to turn off PTH, and lower inflammation. (even up to 1.5:1 or 2:1 is good)
When metabolism is low, the organism is stuck in excessive glycolysis (lactic acid production) which opposes oxidative metabolism (carbon dioxide production).
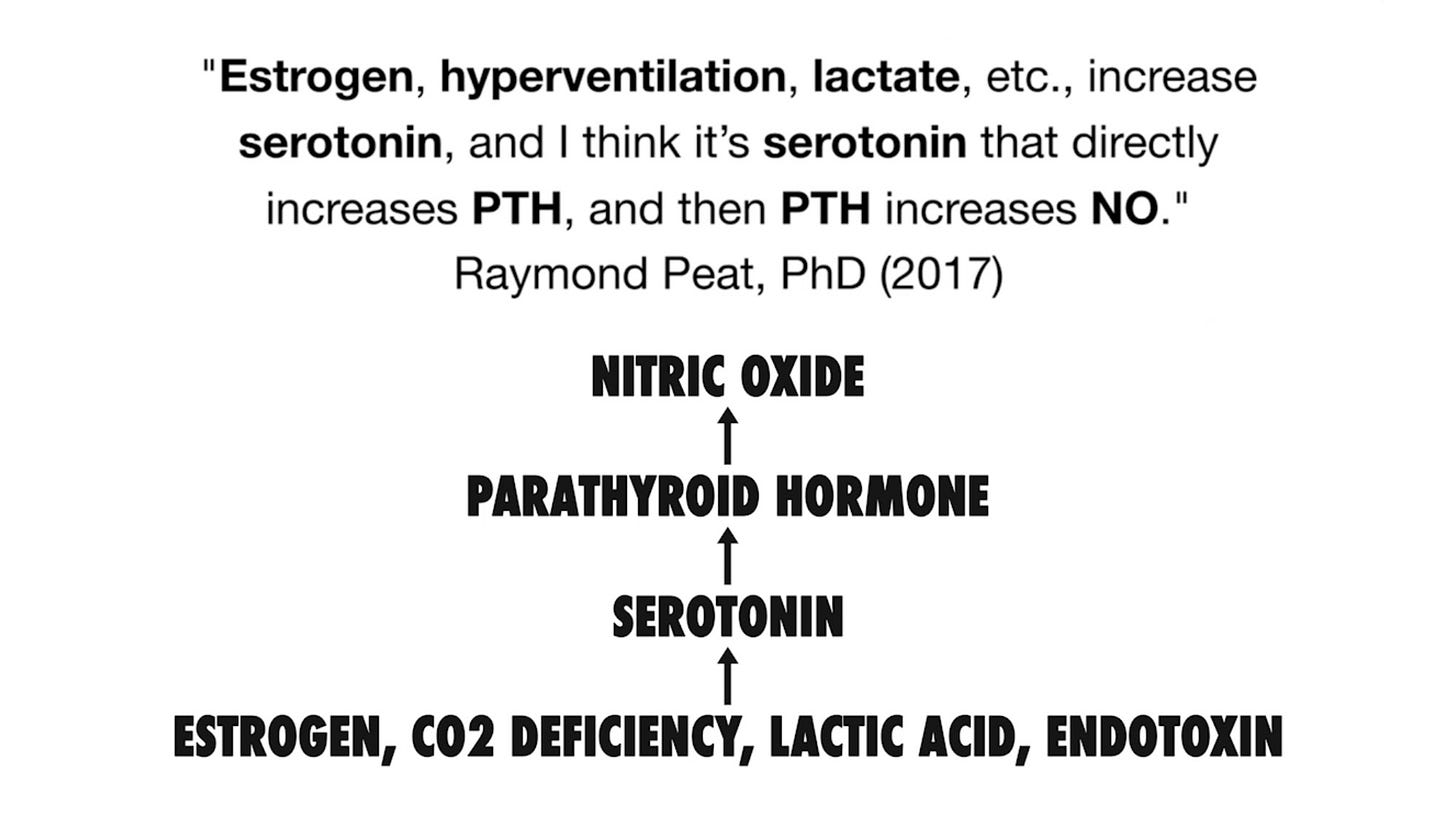
Estrogen and serotonin (promoted by lactic acid) can increase prolactin, PTH, and nitric oxide. These hormones all work together to feed a vicious cycle that impairs energy production.
“PTH (like estrogen and serotonin) inhibits cellular respiration and activates glycolysis, lowering the ATP level and shifting the cells metabolism toward the production of lactic acid rather than carbon dioxide.” -Ray Peat
PTH and stress cause the cell to lose it’s structure, thus allowing calcium (which is normally extracellular) inside the cell. Calcium flooding into the cell causes over-excitation and activates nitric oxide and glutamate which impair mitochondrial respiration and serve as an early step in cell death.1
Calcium and sodium are normally extracellular ions (or electrolytes) and magnesium and potassium are intracellular. When energy is high, this ion balance is properly regulated.
When energy is low, cells tends to lose potassium and magnesium, and take up calcium and sodium.
ATP is what polarizes the cell, meaning it sustains the protein water solute structure that absorbs potassium and magnesium and excludes calcium and sodium.
Heavy Metals
Another harm of dietary calcium deficiency and PTH is that this causes heavy metals to be drawn into the cell; maybe most notably iron, aluminum, and lead which are all involved in aging and degeneration.
Again, lactic acid production is what works together with PTH to liberates calcium from the bones. This also happens to increase intracellular pH, depolarize the cell and increase it’s affinity for metals with a positive charge, such as ionized calcium, iron, aluminum, lead.
Calcium can in essence inhibit heavy metal absorption, providing even more reason to ensure adequate dietary consumption.2
Calcification, Hair Loss and Hypertension
One of the harmful effects of PTH is that it can cause soft tissue calcification due to it’s ability to draw calcium out of the bones.
Calcification is the process where calcium builds up in soft tissues (such as arteries, organs, hair follicles and other tissues) causing the tissue to harden. All of these are places where calcium does not belong.
In my current estimation, calcification can be seen as a way that the organism cuts off energy flow to prevent the stress of functioning when energy is compromised.
Dr. Peat and Georgi Dinkov had an absolutely amazing discussion surrounding calcification on this Generative Energy episode (also in the footnote).
“Intense calcification will cut off an area, turn it to stone, and the process of aging is very, very slow turning to stone. It involves calcification but in a diffuse way that increases inflammation as it lowers function. But the whole organism goes down more or less in a coordinated way rather than calcifying your ears, or your pituitary, or some particular tissue.” -Ray Peat3
Aging can be seen as the process of accumulation of stress, so one thing that we could do to combat this should be to slow and prevent the process of soft tissue calcification as much as possible by consuming enough dietary calcium, thus keeping PTH low and supporting oxidative energy production.
Hair Loss
Parathyroid hormone and it’s role in hair loss is something serious to be considered.
Part of the bioenergetic view of hair loss could involve PTH working together with the other stress mediators to lead to inflammation and eventual calcification of the hair follicles as a physiological response to a low energy environment.
“In vitro experiments with hair follicles show that parathyroid hormone ends the growth cycle. Prostaglandin D2, associated with hair loss, is released from mast cells, and parathyroid hormone is an activator of mast cell degranulation. Hair growth has a 24 hour cycle, and the long cycle of hair shedding and renewal seems to be regulated by the genes involved in the daily cycle (Lin, et al., 2009). It's possible that the daily cycle of parathyroid hormone is responsible for progressive hair loss, as it is for progressive loss of calcium from the bones; many people notice a copious loss of hair mainly in the morning. If this is the case, then a glass of milk at bedtime might have the same protective effect on hair loss that it has on bone loss. Hair loss, like obesity or hypertension, should be taken seriously, as an indication of a systemic metabolic problem.” -Ray Peat4
When energy is deficient and stress is high, resources may be directed away from the less vital systems (such as the hair), and the self-reinforcing stress mediators (such as PTH, cortisol, adrenaline, estrogen, prolactin, serotonin, nitric oxide, aldosterone) could fuel this cycle when elevated chronically.
Hypertension
It was commonly believed that sodium was the main cause of high blood pressure, but Dr. Peat references the work of David McCarron who suggests that calcium deficiency, not sodium excess, is what actually causes high blood pressure.5
Consuming enough calcium in the diet can actually help to lower blood pressure by lowering calcification, and this is one of the many calcium paradoxes.
EMF
Electromagnetic fields (EMFs) but really any kind of stress, can activate the calcium channels, and are involved in liberating calcium into the cell.
As mentioned previously, intracellular calcium causes overexcitation and leads to the synthesis of nitric oxide.
EMFs cause an increase in intracellular calcium and nitric oxide which work together to cause oxidative stress and damage to the cell.6
Again, consuming more dietary calcium than phosphate can help to prevent these issues and support an overall healthy metabolism in the long term.
Calcium Metabolism
The main regulator of calcium metabolism is carbon dioxide production (oxidative metabolism) which helps to incorporate calcium into the bones where it belongs.
Dietary calcium intake is of course the most vital piece of the calcium paradox, as this prevents calcium from being taken from our body stores for use in the organism.
This is similar to the catabolic process in muscle tissue:
When under stress and nutrient deficiency in the diet (most notably carbohydrate deficiency), the body breaks down its own muscle tissue into glucose to use for energy, but as one could expect, this comes at a huge expense.
Also, Vitamin D, K, and magnesium all help to regulate calcium metabolism on top of dietary calcium consumption, and help to lower PTH.
Vitamin D increases calcium absorption from the diet and vitamin K works in conjunction to help ensure that calcium is shuttled into the bones rather than into arteries or soft tissues.
Magnesium, as well as cyproheptadine are calcium channel blockers, which help to prevent the loss of calcium from bones and prevents influx of calcium into cells.7
Calcium Sources
As far as sources of calcium, dairy is one of the richest sources, but as many of us know, milk and other dairy products can easily cause issues when the gut has been chronically dysregulated.
Eggshell, oyster shell, and coral calcium (all sources of calcium carbonate) are usually well tolerated, but can certainly cause issues, particularly for a person with chronic constipation.
When gut motility has slowed due to low metabolism, pure calcium carbonate can easily slow motility even further.
If you’re looking to find a source of calcium that doesn’t irritate the gut; many cheeses can be extremely rich in calcium, allowing you to receive the benefits of calcium in lower quantities of dairy.
Familiarizing yourself with which forms of dairy you tolerate that are highest in calcium can be extremely beneficial for this reason, so I think it’s important to experiment.
For example, digestibility with grass-fed, A2, raw, homogenized, pasteurized; cow, goat, and sheep dairy products can vary significantly.
I find that cheese (particularly raw sheep cheese) seems to be the most digestible for me, and is also extremely rich in calcium, so again, I don’t even need to eat that much to achieve a solid calcium to phosphate ratio in my diet.
The process of cheese fermentation happens to allow the digestibility to increase drastically. (through several means maybe not even fully understood)
With many cheeses, the lactose content is drastically reduced, and the proteins, fats, and bacterial contents are significantly affected. This goes along with the fact that the calcium content can actually increase significantly.
Some highly digestible low lactose cheeses that I recommend to try:
Along with dairy, well cooked leafy green broth (such as kale, collards, nettle) is another good source of calcium and other nutrients such as potassium, magnesium, and vitamin K.
Personally, I would advise against consuming large amounts of leafy green broth, as they can be anti-thyroid and high in oxalates. (tsp of baking soda with the broth can help combat this)
Further Considerations
Aspirin can help regulate calcium:
“Aspirin inhibits the actions of PTH, helping to prevent the calcification of inflamed tissues, and it inhibits the loss of calcium from bones. Aspirin decreases the release of IL-6.” -Ray Peat
Coffee can help lower phosphate:
“Coffee, besides being a good source of magnesium, is probably helpful for lowering phosphate, by its antagonism to adenosine. (Coulson, et al., 1991).” -Ray Peat
Fructose can help lower phosphate:
“While fructose lowers intracellular phosphate, it also lowers the amount that the intestine absorbs from food (Kirchner, et al.,2008), and the Milne-Nielsen study suggests that it increases phosphate loss through the kidneys. The "anti-aging" protein, klotho, increases the ability of the kidneys to excrete phosphate (Dërmaku-Sopjani, et al., 2011), and like fructose, it supports energy production and maintains thermogenesis (Mori, et al., 2000).” -Ray Peat
Niacinamide and aspirin can help lower phosphate:
“Niacinamide is another nutrient that lowers serum phosphate (Cheng, et al., 2008), by inhibiting intestinal absorption (Katai, et al., 1989), and also by reducing its reabsorption by the kidneys (Campbell, et al., 1989). Niacinamide's reduction of free fatty acids by inhibiting lipolysis, protecting the use of glucose for energy, might be involved in its effect on phosphate (by analogy with the phosphate lowering action of a deficiency of polyunsaturated fatty acids). Aspirin is another antilipolytic substance (de Zentella, et al., 2002) which stimulates energy production from sugar and lowers phosphate, possibly combined with improved magnesium retention (Yamada and Morohashi, 1986).” -Ray Peat
PTH rises at night, calcium before bed can help:
“A deficiency of these has consequences much worse than kidney stones. When vitamin D or calcium is deficient, or when phosphate is excessive, and in hypoglycemia and stress (Ljunghall, et al., 1984), parathyroid hormone increases. This can lead to softening of bones, and hardening of soft tissues, especially arteries, sometimes brain, skin and other organs. Parathyroid hormone increases blood pressure, even before the calcium stiffening is detected. During the night, parathyroid hormone usually rises (Radjaipour 1986; Logue 1989, 1990; Fraser, 1998), and especially during aging, this causes a significant loss of calcium from the bones. Having a large part of the day's calcium at bedtime reduces the nocturnal rise of PTH and calcium loss from bones (Ohgitani, et al., 1997; Mortis, et al., 1997).” -Ray Peat
More Resources on Calcium, Phosphate, and PTH:
https://raypeat.com/articles/articles/calcium.shtml
Ray Peat’s main article on calcium.
https://www.functionalps.com/blog/2011/09/19/calcium-paradox/
This page is a tremendous resource created by Functional Performance Systems regarding calcium with quotes from Dr. Peat, references to his and others work, links to pages FPS has created on subtopics regarding calcium and plenty of research and references.
https://raypeat.com/articles/articles/phosphate-activation-aging.shtml
Ray Peat’s on main article on phosphate.
Takuo Fujita, Japanese physician who was the pioneer of the “Calcium Paradox” and has a tremendous body of work surrounding calcium and PTH.
Fujita’s research is frequently cited in Ray’s work.
https://doi.org/10.1016/j.neuro.2012.11.004 Khandare AL, Ankulu M, Aparna N. Role of glutamate and nitric oxide in onset of motor neuron degeneration in neurolathyrism. Neurotoxicology. 2013 Jan;34:269-74. doi: 10.1016/j.neuro.2012.11.004. Epub 2012 Nov 21. PMID: 23178458.
https://doi.org/10.1046/j.1471-4159.1998.70041541.x McNaught KS, Brown GC. Nitric oxide causes glutamate release from brain synaptosomes. J Neurochem. 1998 Apr;70(4):1541-6. doi: 10.1046/j.1471-4159.1998.70041541.x. PMID: 9523571.
#64:Life |Energy|Estrogen|Fibrosis|Calcification |Process Theology|Altruism with Ray Peat Full discussion starts at 5:43
“Adaptogenic Milk” by Ray Peat (2017)
https://doi.org/10.1016/0002-9343(87)90268-3 McCarron DA, Morris CD, Bukoski R. The calcium paradox of essential hypertension. Am J Med. 1987 Jan 26;82(1B):27-33. doi: 10.1016/0002-9343(87)90268-3. PMID: 3544831.
https://pubmed.ncbi.nlm.nih.gov/3011665/ Ellison DH, Shneidman R, Morris C, McCarron DA. Effects of calcium infusion on blood pressure in hypertensive and normotensive humans. Hypertension. 1986 Jun;8(6):497-505. doi: 10.1161/01.hyp.8.6.497. PMID: 3011665.








Awesome post!! I’ll definitely be looking back on it to help crystallize my understanding and application of this knowledge!
Thank you - what a great post.